|
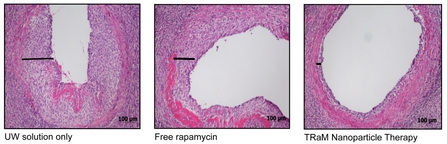
TRaM therapy in aorta transplants
|
Modulation of Donor Endothelial-Memory T cell Interactions Organ transplantation has become an accepted modality for the treatment of end-stage organ failure. The field of transplantation has made tremendous strides within the last thirty years, allowing for newer, more potent immunosuppressive medications rendering acute rejection episodes less frequent and less aggressive. In spite of these accomplishments, transplant recipients continue to succumb to the systemic side effects of standard immunosuppression, including fatal cancers and infections.
We have created a micellar device, both Targeted (TRaM) and untargeted (RaM), at a size conducive to therapeutic delivery and cellular uptake. Tracking fluorophores allow us to detect and monitor the delivery. Focused delivery is achieved by decorating the nanoparticle with various targeting molecules. Local rupture of the device allowing for delivery of the payload has been programmed into the device such that release of a particular therapy is dependent on the environment specific to the transplanted organ. Promising proof-of-concept suggest that these devices improve the patients ability to maintain tolerance to and keep their organs without causing immunosuppression over their entire immune system. |
Breaching the Blood Brain Barrier to Treat Glioblastomas
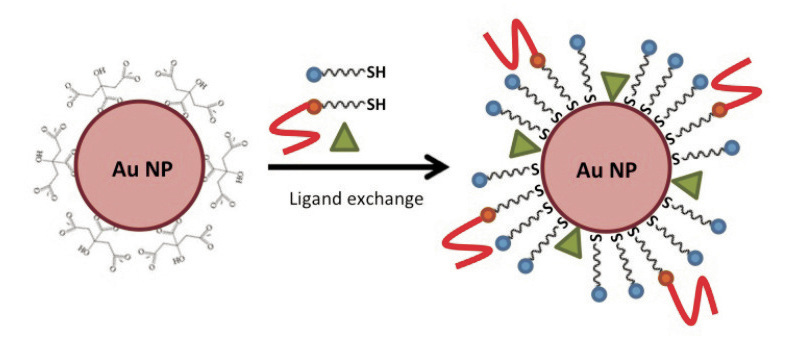
Brain cancer is a life-threatening disease in which only a minority of patients is likely to survive. Late diagnosis and limitations of conventional therapies, as a result of inefficient delivery and non-specificity to brain tumors, are among the major reasons for this unsolved problem. Multi-functional NP drug vectors provide a promising platform technology that will enable the targeted delivery of combined diagnostic and therapeutic agents for cancer treatment. The development of therapeutic NP conjugates with specific tumor targeting and an increased therapeutic index will allow for the treatment and post-therapy monitoring of brain cancers.
Nanoparticle-based delivery has emerged as a promising approach to improve the targeting and efficacy of photosensitizers, such as phthalocyanines (Pc 4), for photodynamic therapy (PDT). Factors that directly impact PDT are the location and concentration of the photosensitizer and the continued availability of molecular oxygen. This is especially challenging in the treatment of brain tumors as the blood brain barrier (BBB) impedes accumulation of systemically administered photosensitizers and what little drug does diffuse across the BBB is absorbed in both normal and cancerous cells. Nanoparticle platforms have the advantage of integrating multi-functionality for synergistic cancer detection, diagnosis and treatment. |